Photo by the author
Population aging in Brazil is a fact. Chronic degenerative conditions demand changes in the care process. The training of health professionals, especially doctors, is still fragile. The Federal Council of Medicine (CFM) in 2018 identified that only 1,817 physicians were registered as geriatric specialists. At this time, 165 vacancies were also offered for residency programs in geriatrics in Brazil, with a 50% occupancy rate. In addition to this, there is a network of care that is not articulated and that is further divided with the care of communicable diseases. The continuous and permanent education of professionals working in Primary Health Care (PHC) is essential to developing a care network for the elderly population.
The matrix support is described as:
A “Way of producing health in which two or more teams, in a process of shared construction, create a proposal for pedagogical and therapeutic intervention” 1.
A Matrix support is considered an important device for co-responsibility of care and establishment of networks. Two types of teams are identified: the reference and matrix support teams. The reference team: responsible for coordinating and conducting cases, in a longitudinal manner, with health responsibility and building a bond; and, the matrix support: operate as a specialized rearguard, assisting with the handling of cases in a shared and dialogical way, expanding the care repertoire of the professionals of the reference team2.
Matrix support works in two dimensions. Assistance is focused on direct actions with service users, based on the demands identified in the shared spaces; and, technical-pedagogical directed to reference teams, of educational support, to expand their technical capacity and shared case management2.
Therefore, the matrix support of family health teams (FHS) is a strategy, because of the small number of geriatric specialist professionals and the importance of working with the elderly population in the community. These facilitator actions are described in the Entrustables Professionals Activities (EPAs)3 for the formation of the specialist in geriatrics and contribute to the care of the elderly in the community as proposed in the National Health Policy for the Elderly4.
Objective
To develop co-management care work between primary and specialized care; involve geriatric residents in the process, develop skills to articulate care with the network, identify the network available in the construction of a therapeutic plan; train doctors and residents of the FHS in the care of the elderly with complex cases, seek unique therapeutic plans based on the identified demands.
What Was Made
The work started in November 2016 with meetings with the municipal management, unit coordination, and scheduling of team meetings. Their aim was to present the proposal, get to know the teams, raise their problems in caring for the elderly, identify the risk recognition in each team, and schedule shared visits or consultations. Four meetings were held. Home visits and consultations started in January 2017. A questionnaire was proposed to be applied to all the elderly (60 or more) in the territory by community health agents, composed of questions to identify the risk of frailty (PRISMA7)5, and, established participation in one meeting per month with each team, with the objective of discussing and monitoring complex cases, scheduling consultations or home visits, and decide on forward co-management within the geriatric service.
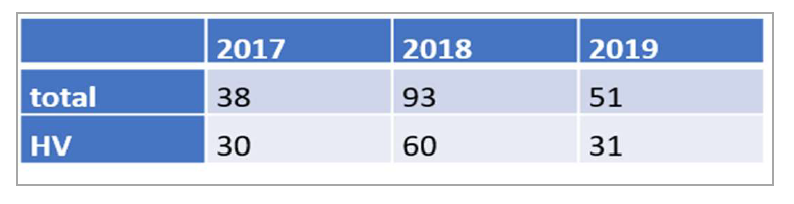
The recognition of the elderly in the territory (1,501 elderly registered in the unit), identification of fragility risk was carried out (450 questionnaires were applied, with risk identified in 107, also 100 elderly were identified as homebound). 182 consultations were made, 121 of which were home visits (Table 1).
Table 1: Consultation and Home Visits (HV)Per Year

Photos by the author
Our visits in Google maps: Figure 1

On the elderly day of the 2019 vaccination campaign, an active search was carried out with the application of PRISMA 7 among 204 elderly people in the community.

Photo by the author
In 2019 we also held a meeting to discuss elderly abuse with community heath agents, because this issue is challenging for them since these professionals’ work involves visiting families in their homes.
Results
The demands for building a proposal in conjunction with the teams were identified: the process of identifying elderly people at risk is not clear to the teams, the frequency of visits by professionals does not follow therapeutic planning based on demands and needs, resolvability is compromised by the lack of longitudinal follow-up of cases, and social risks are very significant and require a specific approach.
The evaluation carried out by the unit's coordination, that was answered by three professionals (from a total of six) where the displacement difficulty, low education, violence in the elderly; and, the lack of knowledge in the area and the short time for consultation are all difficult factors. Positive factors included support for complex cases, an expanded view, and a better understanding of care by professionals.
In the annual evaluation of the residency training, four students reported. Among these, the importance of the work of community agents and the team in caring for the elderly was pointed out, along with the importance of the formation of home visits, in the understanding of the social and health context, as well as in contact with reality, the overload of the team in their daily practice which makes it difficult to work with the elderly, where priority is not identified along with the outcome of consensual interventions with the teams.
Conclusion
This is a rich scenario for the training of specialists and allows for the proposition of strategies for the organization of the care network from Primary Health Care as the organization of the work process, based on the identification of risk, with the establishment of lines of care , based on the identified demands, including planning home visits, proposing criteria for the referral to the geriatric services, and result indicators (vaccination, falls in 12 months, number of medications in use, percentage of elderly mapped in the identification of risk, number of referrals to specialty, number of home visits).
Works Cited
1- Guia prático de matriciamento em saúde mental / Dulce Helena Chiaverini (Organizadora) ... [et al.]. [Brasília, DF]: Ministério da Saúde: Centro de Estudo e Pesquisa em Saúde Coletiva, 2011.
2- Avaliação compartilhada do cuidado em saúde: surpreendendo o instituído nas redes /organização Laura Camargo Macruz Feuerwerker, Débora Cristina Bertussi, Emerson Elias Merhy. - 1. ed. - Rio de Janeiro : Hexis, 2016.
3-Leipzig RM, et al. Geriatric Academic Programs End-of-Training Entrustable Professional Activities for Geriatric Medicine. J Am Geriatr Soc 62:924–929, 2014
4- Brasil, 2006. Política Nacional de Saúde da Pessoa Idosa.
5- Raîche M, Hébert R, Dubois M-F. Guide d’utilisation du questionnaire PRISMA-7 pour le repérage des personnes âgées en perte d’autonomie modérée à grave. Dans Hébert R, Tourigny A, Gagnon M. Intégrer les services pour le maintien de l’autonomie des personnes. Québec, Edisem, 2004; pp 153-175.
Author bio

Luciana Branco da Motta M.D, M.Sc, Ph.D. in Public Health is the Geriatric Service and Residency Program Coordinator at the Rio de Janeiro State University Hospital. She has worked as a geriatrician since 1991and completed her Fellowship in Medical Education from FAIMER Brazil in 2009. Branco da Motta can be reached at This email address is being protected from spambots. You need JavaScript enabled to view it..