Executive Summary
Bucks County, a Pennsylvania Behavioral HealthChoices Primary Contractor for Medicaid, Magellan HealthCare, Inc., the subcontracted Behavioral Health Managed Care Organization (BH-MCO), and Bucks County Mental Health and Drug and Alcohol Outpatient agencies have made a commitment to provide timely access to quality outpatient behavioral health services for Bucks County individuals of all ages. As healthcare evolves and the need for behavioral health services grows stronger, there is a need for data driven outcomes that showcase value. Throughout the last year, select outpatient agencies have worked with Bucks County and Magellan HealthCare, along with a national consultant, to identify areas of opportunity within their organization and make vital shifts in their agency culture to produce quality outcomes. Within this collaborative process between public, nonprofit, and for profit entities, each organization has demonstrated the ability to evolve and continually improve to a future of Value Based Purchasing.
Description of the Initiative
Bucks County, as a Pennsylvania Behavioral Health HealthChoices Contractor, and the subcontracted BH-MCO, Magellan Healthcare, Inc., implemented a program in 2011 to improve access to Outpatient Services and treatment quality. This program involved a strong oversight and monitoring component with frequent provider meetings, access data collection, and clinical record auditing. During Phase 1, advancement was fostered in the areas of clinical supervision and training, trauma informed care, peer support, integrated physical and behavioral health coordination, identification of co-occurring disorders, and tobacco dependence treatment. Despite these successes, challenges in ongoing access quality measures continued. Periodic review of process data included access to initial assessment, length of time from assessment to first clinical appointment, and access to psychiatric care once recommended. Improvement was seen over time in access to initial assessment. However consistent improvement in reducing the length of time from assessment to first clinical appointment as well as timely access to a first Psychiatric visit was not found. Additionally, enhanced quality and access to treatment is expected to improve treatment engagement, and community tenure, and reduce utilization of Mental Health (MH) hospitalization. Unfortunately, positive impact on cost of care for MH Inpatient care was not discerned, and the state targets for seven- day follow-up treatment appointments after MH Inpatient discharge and 30-day MH Inpatient Readmission rates have not been met.
Recognizing that a change in the program model was needed, a growing interest in Value Based Purchasing (VBP) in the Behavioral Health marketplace at the national and state level in Pennsylvania was noted. This seemed the opportune time to prepare our Mental Health and Substance Use serving Outpatient network of providers for the future marketplace. This could be utilized toward further change in access to care, service quality, and treatment outcomes. The intent was to move from this Phase 1 process oriented model of oversight toward, to a Phase 2 educational transition period with increased provider collaboration, toward an outcome, quality focused approach at Phase 3. As such, a core group of providers agreed to collaborate with Bucks County and Magellan Healthcare in developing a pilot outcomes-based approach to effect sustained, systemic change.
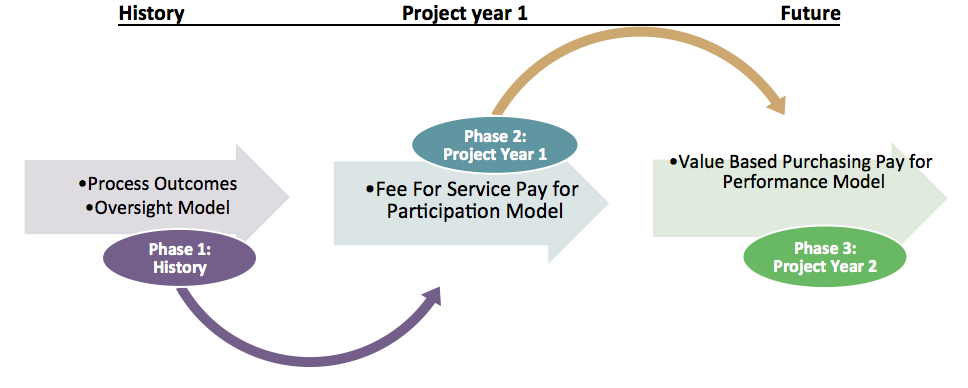
This strategic 3 phase plan differed from our existing HealthChoices contracted models by moving the emphasis from an oversight focus to a more independent ‘Pay for Participation’ approach in an effort to shift the Outpatient Behavioral Health system toward a VBP model. Contracts were drawn with providers to participate in this quality improvement process. Outpatient is a HealthChoices Medicaid In-Plan service and the in-network provider agencies are funded ongoing for provision of clinical services. These identified providers earned bonuses for participation in trainings and implementation of their self-driven pilot project plan.
During Phase 2, Project Year 1, which began July 1, 2016, the focus has been to assist participating providers in creating a structure for identifying and implementing quality improvement processes and in making data driven decisions. The Bucks County Department of Behavioral Health contracted with the National Council for Behavioral Health for their technical assistance in moving the Outpatient system from a process oriented approach to a performance oriented model. Training and technical assistance were offered through a collaborative effort to support providers in this transition. Each provider agreed to create a quality improvement process within their own agency by developing and executing a rapid cycle improvement pilot project. These projects aimed to positively impact 1) their organization’s functioning and internal improvement goals, and 2) the local Behavioral Health system of care as a whole through various measures.
The Bucks County Department of Behavioral Health and Magellan Healthcare offered the Outpatient providers a ‘Pay for Participation’ structure that incentivized the achievement of key benchmarks within their projects which include: 1) Identification of a Quality Leadership Team, 2) Participation in two cross-agency Quality Improvement trainings, 3) Submission of a proposal including an Executive Summary, Work Plan, and Communication Plan, 4) Participation in Consultation Calls with progress reports and 5) Submission of a final Project Summary. Each participating agency was assessed on an ongoing basis as projects were designed and implemented, and interventions were refined.
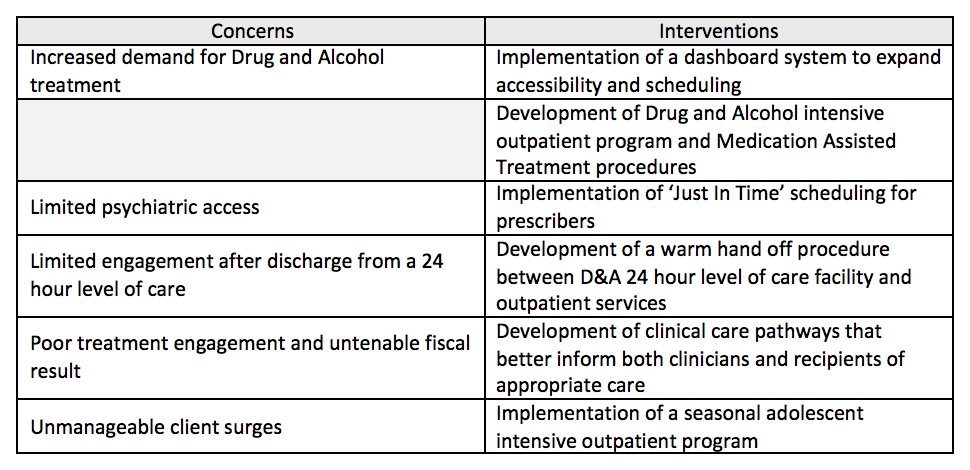
The provider- specific projects varied in content and sought to address the following concerns:
Positive effects of the quality improvement work were reported by agencies related to organizational functioning and moving toward internal improvement goals. These vary across providers but include:
- A substantial decrease of wait list for drug and alcohol services
- A new intensive outpatient program in our network
- Improved use of workflows
- Enhanced coordination of services
- A paradigm shift to the use of a research-informed approach
- More use of evidence based and evidence informed practices
- Improved psychiatric access for scheduled appointments from 19 days to nine days and better scores on Difficulties in Emotion Regulation Scare (DERS) for adolescents completing an intensive outpatient program.
- As an adjunct to one pilot project, an agency achieved gaining a memorandum of understanding with a nearby university to implement a psychiatric residency program within their outpatient facility.
As the pilot projects continue, we anticipate more quantitative results to align with goals of our Behavioral Health Outpatient system of care.
During Phase 3, Project Year 2 (July 2017-June 2018), provider interventions will be evaluated for impact on the following interim performance outcomes: 1) 7 Day Follow Up after MH Hospitalization, 2) 30 Day Readmission to MH Hospitalization, 3) Initiation and Engagement for AOD diagnoses. To help guide development of performance measures for VBP, provider and service recipient meetings will be held by Bucks County and Magellan HealthCare to gain stakeholder insight regarding quality treatment and defining value.
At the end of Year 2, a VBP model will be implemented by Magellan Healthcare, wherein performance is assessed against specific targets via an Outpatient Scorecard with reimbursements aligned to those outcomes. The implementation of this is anticipated by the close of 2018.
The overarching goals of a Value-Based Purchasing model and collaborative approach are to develop a high-performing, high-value network, customized to Outpatient services in our community. Providers will become increasingly cost efficient and will offer better quality and focused interventions for individuals. Currently, system level performance measures for Outpatient VBP are under development. However, the process of enlisting provider engagement has promoted improved collaboration between providers, Bucks County, and our BH-MCO, and has resulted in a community of providers who have increased ability to implement Quality Improvement practices to aid their eventual and ongoing success in the VBP market.
Author Bios
Susanne Ohama is a Licensed Psychologist and Clinical and Quality Manager for Bucks County Behavioral Health, a primary HealthChoices Medicaid Contractor with PA OMHSAS. With over 30 years in the public behavioral health arena, a focus has been to improve the behavioral health system to better help individuals and families lead more satisfactory lives.
Dana Lombardi is a Licensed Professional Counselor and Project Manager working for Magellan Healthcare. She has worked in the behavioral health system for 10 years with experience in children and family services, case management, and outpatient programming. She is dedicated to improving the quality of care for individuals within the public healthcare system.


